MRI Predicts Survival in Locally Advanced Rectal Cancer
By MedImaging International staff writers
Posted on 12 Sep 2011
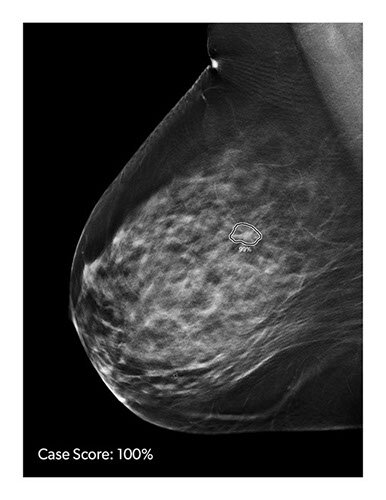
A new study has shown that magnetic resonance imaging (MRI) used to assess responses to presurgery (neoadjuvant) chemotherapy or radiation may predict survival among patients with advanced rectal cancer. The findings suggest that MRI-evaluated tumor responses to neoadjuvant therapy could help clinicians to plan their patients’ subsequent treatments better.Posted on 12 Sep 2011
MRI prior to surgery could help in the management of patients in a number of ways, including offering more intense therapy or alternative chemotherapy to those patients who appear initially resistant to chemotherapy, or changing the surgical strategy.
“This is the first time that MRI has been shown to predict outcome for patients with rectal cancer who have completed initial chemoradiation therapy,” said lead author Gina Brown, MBBS, MD, consultant radiologist and honorary senior lecturer in the department of radiology at the Royal Marsden Hospital NHS (National Health Service) Trust (Sutton, UK). “MRI staging and reassessment of rectal cancers before and after chemoradiotherapy are not routinely done for all patients. We’ve shown that using MRI this way can help change the course of patient care, perhaps enabling physicians to choose a more effective chemotherapy drug or even in some cases ultimately avoid surgery.”
In the trial called MERCURY (Measuring Effective Reductions in Cholesterol Using Rosuvastatin therapy), researchers used MRI to measure tumor shrinkage in 111 patients who had previously undergone preoperative radiotherapy or both chemotherapy and radiation (chemoradiation) for locally advanced rectal cancer. The group part of a larger study of MRI use in improving rectal cancer staging begun in 2002 was followed for five years. The researchers measured tumor response in terms of tumor regression grade [TRG], which measures the degree of tumor shrinkage after therapy, and the involvement of circumferential resection margin (CRM), which refers to the remaining cancer at the tumor edges after treatment, or predicted to remain after surgery. Patients were broadly designated either a “good” or “poor” responder to chemoradiation, according to MRI, and researchers compared survival of the two groups.
Investigators discovered that 72% of good responders to chemotherapy/radiation were alive after five years compared to 27 % of those who were poor responders. The disease-free survival for those with good responses was 64% versus 31% for the poor responders. Moreover, local recurrence rates at five years for those patients for whom there was MRI-predicted CRM involvement was 28% compared to 12% for patients with predicted cancer-free tumor margins.
Rectal cancer is typically found in advanced stages, and as a result, neoadjuvant chemoradiation is frequently given to try to shrink tumors and make them easier to remove. While surgeons attempt to completely remove the cancer in order to minimize the chances of cancer returning, advanced tumors are more difficult to completely remove and more likely to have unseen cancer remaining at the edges of tissue at the surgery site. A positive surgical margin (tumor that remains at the borders of the surgical resection) is considered a strong predictor of local recurrence.
Of the 111 patients in the study, 73% (81 patients) were expected to have cancer left in the surgical margins prior to initial treatment. After neoadjuvant therapy, only 42% (47 patients) were predicted to have disease left in the surgery margins, meaning this group was still at risk for recurrence prior to surgery.
“The next step is to take these tumor response grades and decide what the best treatment approach could be based on the degree of responses,” Dr. Brown said. She noted that future trials investigating neoadjuvant chemotherapy followed by chemoradiotherapy might be able to identify a subgroup of patients that has a good response and for whom chemotherapy alone might be enough, while also identifying those who needed further therapy prior to surgery. In some instance, the preoperative treatment removed all evidence of the tumor, leading some physicians to question the need for surgery.
The investigators have started a trial to study what occurs to those individuals who appear to not have any remaining cancer with chemoradiation alone and have deferred surgery. In some cases, this has resulted in long-term deferral with anal sphincter preservation. Other trials may also be designed to use MRI results in regard to treatment efficacy.
Related Links:
Royal Marsden Hospital NHS Trust