Artificial Intelligence Accurately Predicts Radiation Treatment Side Effects
|
By MedImaging International staff writers Posted on 01 Oct 2019 |

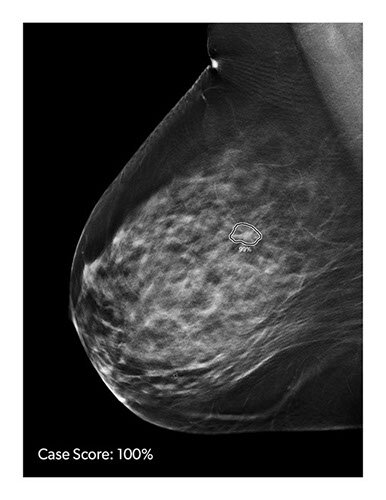
Image: New research has shown that a computer model can predict side effects associated with radiation therapy (Photo courtesy of Technology Networks).
Researchers from the University of Texas MD Anderson Cancer Center (Houston, Texas, USA) have demonstrated that a sophisticated computer model can accurately predict two of the most challenging side effects associated with radiation therapy for head and neck cancer. This precision oncology approach has the potential to better identify patients who might benefit from early interventions that could help prevent significant weight loss after treatment or reduce the need for feeding tube placement.
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
Latest Industry News News
- Bayer and Google Partner on New AI Product for Radiologists
- Samsung and Bracco Enter Into New Diagnostic Ultrasound Technology Agreement
- IBA Acquires Radcal to Expand Medical Imaging Quality Assurance Offering
- International Societies Suggest Key Considerations for AI Radiology Tools
- Samsung's X-Ray Devices to Be Powered by Lunit AI Solutions for Advanced Chest Screening
- Canon Medical and Olympus Collaborate on Endoscopic Ultrasound Systems
- GE HealthCare Acquires AI Imaging Analysis Company MIM Software
- First Ever International Criteria Lays Foundation for Improved Diagnostic Imaging of Brain Tumors
- RSNA Unveils 10 Most Cited Radiology Studies of 2023
- RSNA 2023 Technical Exhibits to Offer Innovations in AI, 3D Printing and More
- AI Medical Imaging Products to Increase Five-Fold by 2035, Finds Study
- RSNA 2023 Technical Exhibits to Highlight Latest Medical Imaging Innovations
- AI-Powered Technologies to Aid Interpretation of X-Ray and MRI Images for Improved Disease Diagnosis
- Hologic and Bayer Partner to Improve Mammography Imaging
- Global Fixed and Mobile C-Arms Market Driven by Increasing Surgical Procedures
- Global Contrast Enhanced Ultrasound Market Driven by Demand for Early Detection of Chronic Diseases
Channels
Radiography
view channel
Novel Breast Imaging System Proves As Effective As Mammography
Breast cancer remains the most frequently diagnosed cancer among women. It is projected that one in eight women will be diagnosed with breast cancer during her lifetime, and one in 42 women who turn 50... Read more
AI Assistance Improves Breast-Cancer Screening by Reducing False Positives
Radiologists typically detect one case of cancer for every 200 mammograms reviewed. However, these evaluations often result in false positives, leading to unnecessary patient recalls for additional testing,... Read moreMRI
view channel
PET/MRI Improves Diagnostic Accuracy for Prostate Cancer Patients
The Prostate Imaging Reporting and Data System (PI-RADS) is a five-point scale to assess potential prostate cancer in MR images. PI-RADS category 3 which offers an unclear suggestion of clinically significant... Read more
Next Generation MR-Guided Focused Ultrasound Ushers In Future of Incisionless Neurosurgery
Essential tremor, often called familial, idiopathic, or benign tremor, leads to uncontrollable shaking that significantly affects a person’s life. When traditional medications do not alleviate symptoms,... Read more
Two-Part MRI Scan Detects Prostate Cancer More Quickly without Compromising Diagnostic Quality
Prostate cancer ranks as the most prevalent cancer among men. Over the last decade, the introduction of MRI scans has significantly transformed the diagnosis process, marking the most substantial advancement... Read moreUltrasound
view channel
Deep Learning Advances Super-Resolution Ultrasound Imaging
Ultrasound localization microscopy (ULM) is an advanced imaging technique that offers high-resolution visualization of microvascular structures. It employs microbubbles, FDA-approved contrast agents, injected... Read more
Novel Ultrasound-Launched Targeted Nanoparticle Eliminates Biofilm and Bacterial Infection
Biofilms, formed by bacteria aggregating into dense communities for protection against harsh environmental conditions, are a significant contributor to various infectious diseases. Biofilms frequently... Read moreNuclear Medicine
view channel
New SPECT/CT Technique Could Change Imaging Practices and Increase Patient Access
The development of lead-212 (212Pb)-PSMA–based targeted alpha therapy (TAT) is garnering significant interest in treating patients with metastatic castration-resistant prostate cancer. The imaging of 212Pb,... Read moreNew Radiotheranostic System Detects and Treats Ovarian Cancer Noninvasively
Ovarian cancer is the most lethal gynecological cancer, with less than a 30% five-year survival rate for those diagnosed in late stages. Despite surgery and platinum-based chemotherapy being the standard... Read more
AI System Automatically and Reliably Detects Cardiac Amyloidosis Using Scintigraphy Imaging
Cardiac amyloidosis, a condition characterized by the buildup of abnormal protein deposits (amyloids) in the heart muscle, severely affects heart function and can lead to heart failure or death without... Read moreGeneral/Advanced Imaging
view channel
New AI Method Captures Uncertainty in Medical Images
In the field of biomedicine, segmentation is the process of annotating pixels from an important structure in medical images, such as organs or cells. Artificial Intelligence (AI) models are utilized to... Read more.jpg)
CT Coronary Angiography Reduces Need for Invasive Tests to Diagnose Coronary Artery Disease
Coronary artery disease (CAD), one of the leading causes of death worldwide, involves the narrowing of coronary arteries due to atherosclerosis, resulting in insufficient blood flow to the heart muscle.... Read more
Novel Blood Test Could Reduce Need for PET Imaging of Patients with Alzheimer’s
Alzheimer's disease (AD), a condition marked by cognitive decline and the presence of beta-amyloid (Aβ) plaques and neurofibrillary tangles in the brain, poses diagnostic challenges. Amyloid positron emission... Read more.jpg)
CT-Based Deep Learning Algorithm Accurately Differentiates Benign From Malignant Vertebral Fractures
The rise in the aging population is expected to result in a corresponding increase in the prevalence of vertebral fractures which can cause back pain or neurologic compromise, leading to impaired function... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more